

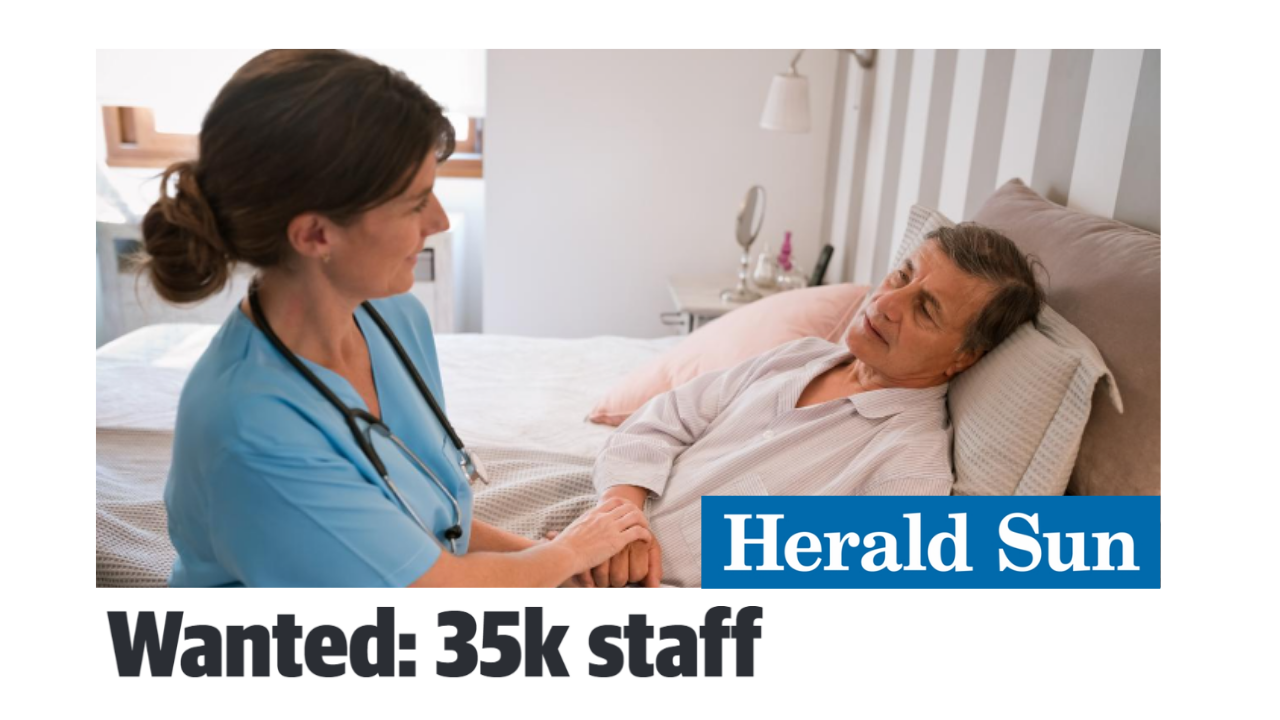
When CEDA last looked at the aged care workforce, we forecast there would be a need for an additional 17,000 direct care workers each year over the coming decade. Less than a year later, this annual shortfall has doubled due to a combination of challenging circumstances and a lack of action. Now we are expecting an annual shortfall of 30,000 to 35,000 direct care workers.
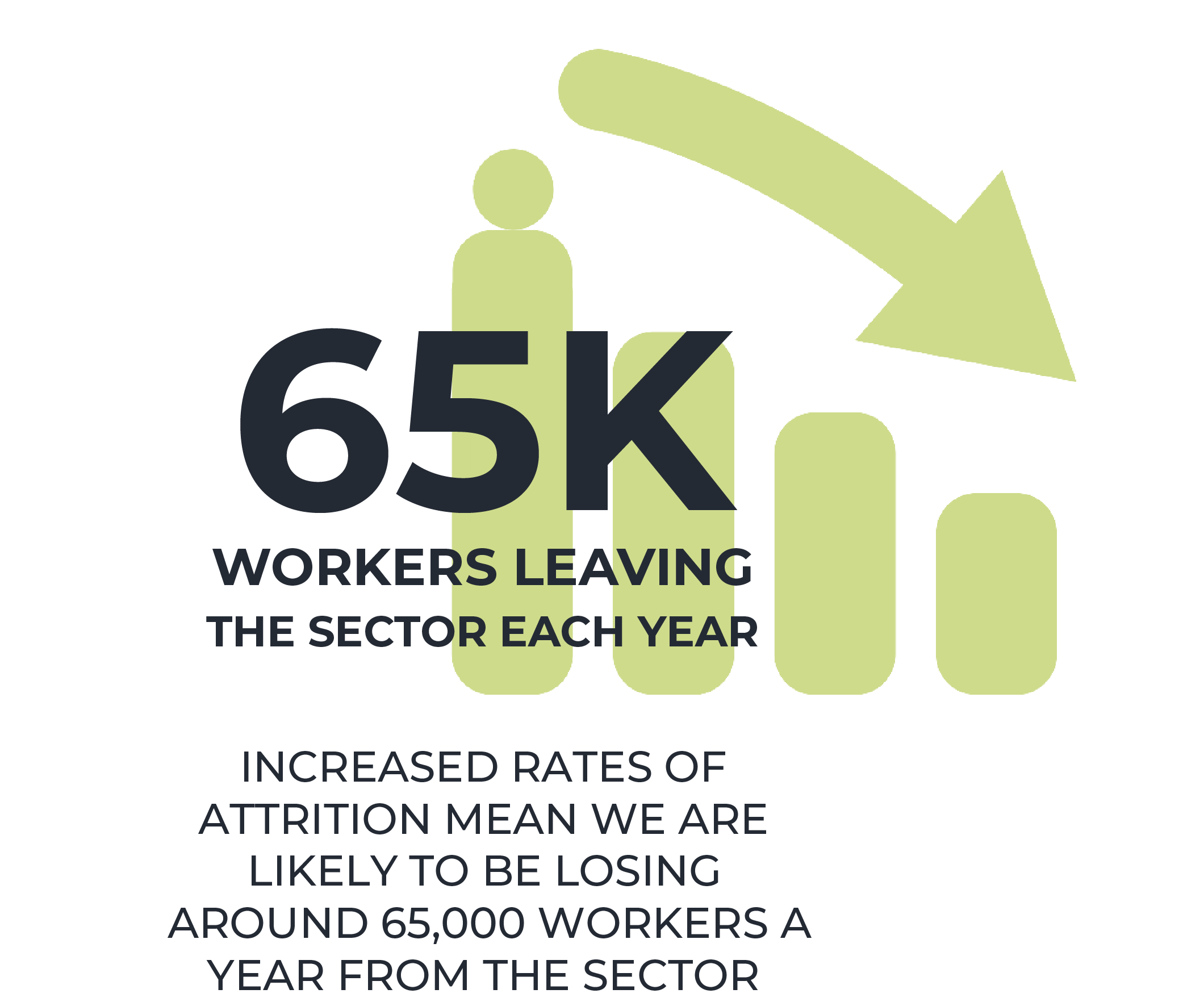
If workforce shortages at this level continue, we will not have enough workers to meet the basic standards of care recommended by the Royal Commission.1 Miniscule levels of migration and increased levels of attrition in the sector, estimated to be around 65,000 workers a year, have exacerbated existing shortages. This is no longer a problem for the future, it is a critical issue that needs to be tackled immediately.
This paper updates the workforce projections of CEDA’s Duty of Care report, released in August 2021, based on the latest information and industry consultation. It finds that filling the growing shortfall in the aged care workforce is a task that is escalating each day. Filling this shortfall will not be achieved without determined and consistent effort. Urgent implementation of the recommendations made in CEDA’s Duty of Care report is necessary.
Improving the quality of care for older generations is a social imperative as well as an economic one. The sector receives more than $22 billion of government funding per year, supports more than 1.3 million people receiving some form of care service and employs more than 360,000 people.2
The new Albanese government has made commitments towards increasing the quality of aged care,3 including 24/7 registered nurses in residential aged care and longer mandated care time. These commitments will be difficult to achieve without a turnaround in the workforce numbers. The new government’s commitment to support and fund a pay rise for aged care workers as part of the Fair Work Commission's work value case is a step in the right direction but pay alone will not be enough to solve the workforce challenge.
What has changed?
The aged care workforce was already under significant pressure with staff shortages, low pay, poor working conditions and increased negative attention through the Royal Commission. Over the past year, these issues have been amplified by the impacts of COVID-19. Aged care has been at the centre of many COVID-19 outbreaks, resulting in even more difficult working conditions and staff themselves becoming sick. For a workforce that was already burnt out prior to COVID-19, this has been the breaking point for many. During a time where unemployment is low, many have chosen to leave the sector.

The Australian Nursing and Midwifery Federation undertook a survey of workers in early 2022 on the impact of COVID-19 on the aged care workforce. It found that 20 per cent of workers intended to leave their employment within the next 12 months, and 38 per cent within the next one to five years.4 The survey also asked workers what the most challenging aspect of dealing with COVID-19 in aged care has been – the answer to this was overwhelmingly staff shortages. A survey done by SkillsIQ of recent students in the aged care space found that 13 per cent of those surveyed planned to train or reskill into another industry directly due to the impact of COVID-19 and/or the 2019-20 bushfires.5
A UTS report into the aged care sector found that staffing levels in residential care remain well below that required to meet the basic standards of care (200 minutes of care per resident per day) that the industry should be working towards. The rate of growth in direct care staffing time has slowed at a time when it should be accelerating. Care time per client in home care has actually decreased – a continuing trend over the past five years. This is attributed to the difficulty in finding workers.6
Some stopgap measures were put in place by the previous Federal Government, including bonus payments (up to a maximum of $800 per worker) and even the Australian Defence Force being deployed to support the aged care workforce during the COVID-19 wave earlier this year. But there has been little to no progress on addressing the underlying factors that are causing the workforce shortages.
Given the immediate nature of the workforce challenge, priority must be given to actions that will boost the workforce in the short term, while continuing to improve longer-term workforce outcomes. This should include the following recommendations from Duty of Care:
How many workers do we need?
Our 2021 research found that Australia needed a net increase of 17,000 direct care workers per year from 2020 through to 2030, and that doing so would require significant changes within the industry.
In the year since the estimate was published, not only has no progress been made, but the circumstances have significantly worsened. Industry consultation suggests that attrition has increased substantially over the past two years, due to staff burnout and the availability of jobs elsewhere. Migration levels have not yet returned to pre-pandemic levels, let alone increased. Training levels have remained relatively steady. If this is not turned around quickly, CEDA’s 2021 forecasts of a cumulative shortfall of 110,000 workers by 2030 will look like a significant underestimate of the workforce shortages facing the sector.
In our previous report we provided a number of scenarios of workforce trends.7 The latest evidence suggests we are tracking towards the worst-case scenarios. The graph below shows the two worst case scenarios from our previous report – one with no workers coming in through migration, and one with more workers leaving through increased attrition.8 These scenarios now reflect current conditions – we are likely somewhere in between the two. Increased rates of attrition mean we are likely to be losing around 65,000 workers a year from the sector. Replacing these people is no easy task and takes up significant time and resources for providers.
With more workers leaving the sector and fewer coming in through migration, the gap between where we need to be to meet demand and where we are currently has essentially doubled. If current conditions continued, we would have a shortfall of around 30,000-35,000 direct care workers a year.
Pay rises are not enough
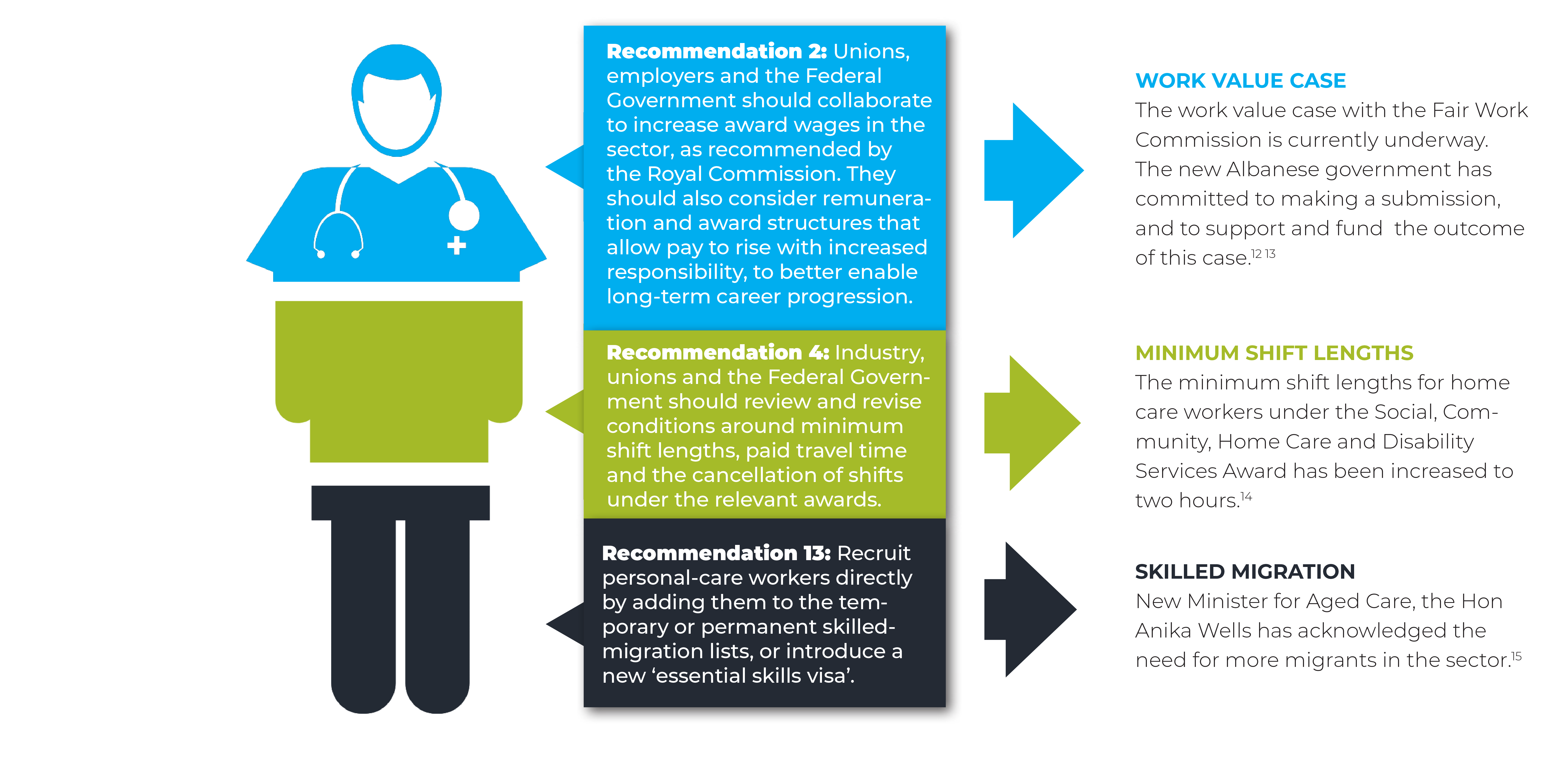
Wages levels and relativities are part of the problem in attracting and retaining workers. Workers in the sector make substantially less than those working in similar roles and with similar qualifications in adjacent industries such as disability and health care. As per our recommendation in Duty of Care, we continue to support unions and stakeholders in working together on the work value case currently before the Fair Work Commission to increase wages in aged care awards.9 The recent decision to increase the modern award minimum wage will benefit many aged care workers but a more substantive increase is still required to bring pay rates into line with adjacent care sectors. The new Albanese government has committed to make a submission to support and fund higher wages in the sector. This is a good first step.
As important as increasing wages is, this alone will not solve the aged care workforce problem. While it may go some way to stemming the tide of workers leaving, the industry must also address other working conditions, such as hours and rostering, training and career progression. CEDA made 18 recommendations in Duty of Care showing the magnitude of the problem means that all levers must be pulled to make headway on this challenge.
The role of migration
Migration is crucial to rebuilding the aged care workforce. Prior to COVID-19, we estimated around 30 per cent (nearly 80,000 workers) of the workforce were migrants. While borders re-opened in 2022, numbers of migrants remain low and visa processing times are long. There is also significant competition for migrants in a range of sectors, which means aged care may miss out. In order to meet the demand for workers, migration will need to return to at least previous levels, if not more. We need to make Australia and the industry more attractive for potential migrants.
Personal care workers, who make up most of the aged care workforce, are not currently eligible for a skilled migration visa. Most of these workers come to Australia on a working holiday, international student or partner visa. Prioritising an essential skills visa would allow these workers to directly enter Australia to work in the industry. This targeted migration would focus on trained and motivated staff who want to work in the sector. There should be a pathway to permanent residency for these workers – as demand for workers in this sector will be with us for the long term. Other countries such as Canada and New Zealand have piloted programs to directly recruit migrant workers for their care sectors.10
We will also need more migration at the registered nurse level. The Albanese government has committed to having 24/7 registered nurses in all facilities. It is difficult to see a pathway to fulfilling this commitment without a significant increase in migration, as acknowledged by the new Minister for Aged Care, the Hon Anika Wells.11

Where to from here?
The situation is not all doom and gloom. Aged care is a rewarding career, with high levels of job satisfaction. If we can start to rebuild the workforce, lift wages and conditions, and improve the reputation of the industry we could see a virtuous cycle where increased attractiveness and job satisfaction encourage more and more people to enter the industry.
But this won’t occur without significant effort. Addressing pay and migration should be the immediate priorities, however we also need to look at improving training options, career pathways and investing in new technologies to improve productivity. By pulling all the available levers we can start to make progress on building the caring workforce that Australia needs to provide the high level of care we all expect for ourselves and our families.
Key recommendations from Duty of Care that have seen some movement:
While there has been no substantial action on the recommendations from Duty of Care, there have been some small movements in the right direction:
CEDA's advocacy on aged care: a timeline
-
2021
-
2021
-
2021
-
2022
-
2022
-
2022
1 https://agedcare.royalcommission.gov.au
3 https://www.alp.org.au/policies/aged-care
5 https://www.skillsiq.com.au/ResourcesResearchandSubmissions/Longitudinalstudy
7 See Appendix A – Methodology and Assumptions in Duty of care for explanation of scenarios and data sources.
8 An attrition rate of 25% is used in this scenario, up from 18% used in the baseline.
9 https://www.fwc.gov.au/hearings-decisions/major-cases/work-value-case-aged-care-industry
10 https://www.canada.ca/en/immigration-refugees-citizenship/services/immigrate-canada/caregivers.html
12 https://www.alp.org.au/policies/aged-care
13 https://www.fwc.gov.au/hearings-decisions/major-cases/work-value-case-aged-care-industry
Images: ilya2k | infogram; Gert Stockmans | Unsplash; Dominik Lange | Unsplash; depotvisual | Envato
Media Mentions

.png?ext=.png)
.png?ext=.png)
.png?ext=.png)
.png?ext=.png)
.png?ext=.png)

.png)

.png)



.png)